The Potential of AI to Enhance Medical Review and Prior Authorization Efficiency
Authors: Prem Sundivakkam, PhD., MBA., BCMAS; Veni Kandasamy, PhD; Poonam Gupta-Krishnan
Health equity, defined as the fair and just opportunity for everyone to attain their highest level of health, is a pressing issue that demands our attention. It necessitates a societal commitment to rectify historical and contemporary injustices, surmount economic and social barriers to health and healthcare, and eradicate preventable health disparities.
The pursuit of health equity is not only a moral imperative but also an economic one. Inefficient resource allocation due to health inequities currently costs approximately US $320 billion and could potentially exceed US $1 trillion in annual spending by 2040 if not addressed. Diseases do not respect borders or socio-economic divides; hence, our efforts to combat them must be inclusive and equitable. By advocating for health equity, we not only uplift the most vulnerable and marginalized but also fortify our global community against future health-related challenges.
The US healthcare system has been plagued by structural inequities since its inception, posing significant challenges to achieving health equity. These inequities are deeply entrenched in societal factors and are reflected in the system’s design, which yields disparate outcomes for different populations. Minoritized populations bear the brunt of these inadequacies, with glaring racial and ethnic disparities in life expectancy, maternal and infant mortality, and numerous chronic diseases.
For instance, diabetes prevalence in the U.S. is highest among American Indian and Alaska Native adults at 13.6%, followed by Black populations at 12.1%, Hispanic populations at 11.7%, Asian populations at 9.1%, and White populations at 6.9%. However, non-White patients are less likely to receive newer, higher-cost drugs and diabetic technology.
Prior Authorization, Medical Review, and Health Equity Amidst Structural Inequities:
The implementation of prior authorization and medical review by health insurance plans can inadvertently intensify health inequities amidst these existing structural inequities. Criticized as a barrier to access, the American Academy of Family Physicians contends that prior authorizations can exacerbate health disparities and create barriers to care for medically underserved patients, patients of color, LGBTQ+ patients, and patients in rural areas.
The stringent cost-control post-authorization processes employed by health insurance plans significantly influence the outcomes of medical reviews, thereby contributing to structural inequities and barriers in the healthcare system. The high cost of the US healthcare system, its most significant weakness, is a prime example. In 2020, national expenditures on healthcare goods and services were approximately $4 trillion, accounting for an estimated 18% of gross domestic product. High care prices largely explain the difference in spending between the US and other developed countries. Moreover, the current US healthcare system often delays or denies high-quality care to those who need it most but can least afford its high cost, leading to avoidable healthcare disparities for people of color and other disadvantaged groups.
Current Challenges in Post Authorization and Medical Review:
The challenges in Prior Authorization and Medical Review includes
- Lack of Transparency: Providers often are uncertain whether a particular recommended treatment requires prior authorization and, if so, which documents the plan requires for approval.
- Inefficiencies in Submission Methods: Plans vary widely on how to format and submit prior authorization requests and supporting documentation.
- Delays in Care: 93% of physicians reported care delays while waiting for health insurers to authorize necessary care.
Opportunities for Improvement using Generative AI:
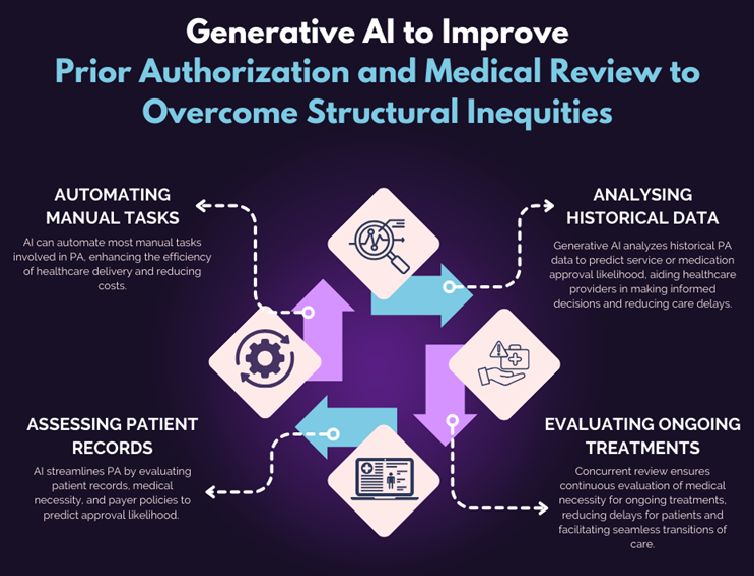
Generative AI can significantly decrease delays in care during the post-authorization and medical review processes. Here are some examples:
- Automating Manual Tasks: AI can automate 50 to 75 percent of manual tasks in the prior authorization process, boosting efficiency, reducing costs, and freeing clinicians at both payers and providers to focus on complex cases and actual care delivery and coordination¹.
- Analyzing Historical Data: Generative AI can analyze historical prior authorization data to identify patterns and predict the likelihood of approval for specific services or medications. This can help healthcare providers make more informed decisions when requesting prior authorization, reducing the likelihood of rejection which can cause delays to patient care⁴.
- Assessing Patient Records: AI can streamline the process by assessing patient records, medical necessity, and payer policies to determine the likelihood of approval. Intelligent prior authorization systems can help providers navigate complex approval requirements, reducing delays and denials.
- Evaluating Ongoing Treatments: By continuously evaluating the medical necessity of ongoing treatments, concurrent review minimizes delays for patients as they are already receiving care, creating more seamless transitions of care.
In conclusion, Generative AI can play a crucial role in reducing delays in care during the post-authorization and medical review processes by automating tasks, analyzing data, assessing patient records, and evaluating ongoing treatments. This can lead to improved patient outcomes and a more efficient healthcare system.
Iyka’s Generative AI Offerings:
About Iyka:
At Iyka’s G19Studio your GenAI solutions extend beyond mere task automation to giving your creativity and decision-making ability a new power to empower your enterprise.
Headquartered in Greater Chicago, Iyka is a leading Digital Transformation, Data management, and data analytics company. Specializing in Data
Iyka provides services through product platforms like- Enterprise-wide unified data discovery platform- Incorta, Health-data-Linkage Platform, Learning Management System,
Awards include the International Best Practices in SME Innovation Award, International Business Leadership Excellence Award, Chicago Daily Herald’s Best Places to Work in Illinois, and Chicago Minority Development Council’s Fastest Growing Minority Company. Iyka’s diversity certifications include MBE, WBE, DBE, 8(a), and WOSB. Master Contracts include: University of Illinois Systems, IPHEC2140, Cook County, State of Illinois, CDW, Federal Aviation Administration (eFAST), and 8(a) STARS III.
For more information visit: www.Iyka.com or call 630-372-3900.